Adelaide & Hills HAND THERAPY
|
'Golfer's Elbow' or Medial Epicondylitis, is a musculoskeletal condition which causes pain on the inside of the elbow.
This pain usually starts around the bony bump which is where the muscles that bend your wrist and fingers come from, and can progress into the forearm muscles. The pain is due to damage to the tendons which attach the muscles to the bone. This damage can be degenerative, in that it can occur over several years, or due to a sudden injury. However is more often due to a change in load to the tendons, for example you decide to take up a new hobby or sport which involves more gripping or wrist bending, and this overloads the tendons. Golfer's Elbow is often confused with Tennis Elbow. Tennis Elbow is a very similar condition, which occurs on the outside of the elbow. Both conditions can be see together, and they are not limited to playing golf or tennis. Golfer's elbow is most often seen in working aged people who have work tasks or hobbies which involve repetitive or prolonged clenching of the fist (gripping) and bending and straightening of the wrist. Some activities which can cause Golfer's Elbow include; painting, hammering, using power tools, playing tennis and golf, even knitting. Symptoms include;
If you think you have Golfer's Elbow, come and see us. We won't give you 'passive' treatments week after week. We will educate you how to manage the symptoms yourself, so that you can spend your time doing the things you enjoy pain free.
0 Comments
Our hands are the tools through which most of us feel and explore the world. Yet, like so many things, most of us take our hands for granted. That is, until they hurt, or stop working properly. That’s when we come to appreciate how precious they are. And when you discover the value of hand therapy. Because of the incredible complexity and importance of the hand; specialty fields of hand surgery and therapy have developed. Most people have never heard of a ‘hand therapist’ before meeting one. But when they need one, and they meet one to know one, they tend to be glad they have. Hand therapists know all about hands, and their job is to get them working again. What is Hand Therapy? Hand Therapy is the rehabilitation of the upper limb, that is, from the fingertip to shoulder and everything in between. Therapy is aimed at reducing symptoms and increasing function, using non-invasive techniques. Meaning therapists don’t operate or prescribe medications. However, they work closely with doctors and surgeons in a team approach. Therapists use specialised tests to assess their clients’ symptoms and determine what the cause may be. They take a history, read any reports and observe the limb, before commencing hands on assessment. Assessment includes feeling (palpating) the skin and underlying muscles, bones etc., and getting the client to perform specific movements. Together this information helps the therapist determine what their symptoms mean. They then work together with clients to set treatment goals, and use specific techniques to help achieve these goals. These include the use of heat and cold, massage, compression, splinting, exercises, education, advice, small aides & equipment, activity and environmental modifications. Who is a Hand Therapist? A Hand Therapist is a registered Occupational Therapist or Physiotherapist who has honed their clinical skills through on the job work. They will have completed extra study, and undertake ongoing professional development to keep abreast of developments in the field. Many countries have a professional association that recognises and represents practitioners. In Australia, we have the Australian Hand Therapy Association (AHTA). Becoming a member of the AHTA is a stringent process. This ensures members are highly skilled in their craft and our profession is respected. Experienced therapists may choose further acknowledgement of their knowledge and obtain the Certified Hand Therapist (CHT, USA) credential. This is an American certification, but highly recognised internationally. Being a CHT demonstrates the practitioner has substantial clinical experience, and advanced theoretical knowledge in hand therapy. Who can Hand Therapy help? Anyone who has had an injury, deformity or disease, in their hands or arms can benefit from hand therapy. Following and injury or operation, hand therapy can assist to manage swelling and scars. Therapists help protect injured structures to optimise healing, before safely working to restore movement and strength. They work with clients to guide them back to using their arm as best they can for work and daily tasks. Hand therapist also help clients who have chronic and degenerative conditions to manage their symptoms. They understand how different diseases effect the body, and how to work with this to maximise participation and independence in valued daily activities. After all, for most of us, our hands play a vital role in enabling us the achieve and enjoy what we most want to from life. So, protect and respect your precious dextrous tools. And in the event, they let you down, rest assured, there is “such a thing as a hand therapist” who can help you get them working again. It might seem unbelievable, but gaming can result in injury! Hand injury that is. And most commonly to the thumb.
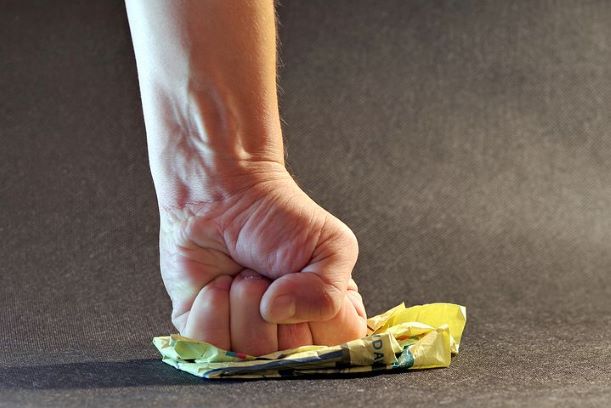
When players become engrossed in a game, it is easy to loose track of time, and become oblivious to strain that play might be having on the body. Injury can result from prolonged play; holding the device in the fingers & thumb for long periods of time, straining the neck and shoulders. Or from rapid & repetitive movements needed to manipulate the console. These actions, over time, take their toll on the tendons which control the thumb. Most commonly resulting in a condition called DeQuervain's tenosynovitis. The tendons at the base of the thumb become swollen and painful, in sometimes can 'creak' or catch during thumb & wrist movement. The sheath surrounding the tendon can also become swollen. People describe a burning pain over the back of the wrist and thumb, often accompanied by swelling. Rest is initially recommended to decrease load on the tendons and reduce swelling. Reducing play or taking a break from gaming will almost certainly help. A splint will support and decrease load on the tendons; allowing for healing. Sometimes a cortisone injection or anti inflammatory drugs are recommended. And in some cases surgery will be required to reduce pressure on the tendons. To prevent Gamer's Thumb, taking regular rest breaks and reducing the time played each session is recommended. Try setting an alarm to remind yourself to stop, rest and stretch- and get in the habit of doing so. Take care of your thumbs, after all, it is said "the thumb is half the hand!" A break in the little finger (5th) metacarpal (hand bone) is often coined a Boxer's Fracture. This is because a common mechanism of injury is from a punching a hard surface with a clenched fist. The bone is usually broken at the neck (close to where the little finger joins the hand) or the base (back of wrist on little finger side of hand).
Pain surrounding the break in the bone and swelling in the region usually occur directly after the blow. However it is important to get an x-ray early, because if the bone has shifted in position it may need an operation to fix it. There is a real chance, that if the bone is left to heal in an incorrect position, that permanent changes in the way the little finger moves will result. A Hand Therapist will make a custom fit thermoplastic splint to protect the bones as they heal, whilst allowing for maximal safe use of your hand. As swelling over the back of the hand is common with Boxer's Fractures, managing swelling is critical, as is getting the healing fracture moving as soon as it is safe to do so. An experienced Hand Therapist can help guide you through this process. Strain to the neck, shoulders, forearms, wrist and hand is not uncommon for musicians who play for prolonged periods of time each week. This usually results from awkward arm or body positioning in handling the instrument or sitting to play. Or overuse of different muscles or tendons from playing for long periods. And can result in aches, pain & swelling in the wrists, forearms and shoulders. In some cases compression on a nerve can cause pins & needles or tingling in the hands can be experienced during or after play.
To help prevent upper limb strain from prolonged play there are some simple and effective things you can do. 1. Warm up before you play Before picking up your instrument or sitting down to play, stretch the muscles of your fingers, wrists, forearms, shoulders & back. By gently stretching the muscles we increase blood flow, this will warm & lengthen the muscles & joints- and help prevent strain. Always move into stretches slowly, and try to hold them for at least 10 seconds each. TIP It can help to start by playing familiar & easier pieces before leading into complex ones. 2. Set a timer, check your posture Getting into the routine of regularly checking your posture can help to prevent strain. Consider setting a timer as a regular reminder. As a general rule it is beneficial to engage your core, relax shoulders, keep neck upright, and relax tight muscle groups. 3. Take a break Factor in regular short rest breaks throughout practice. It is easy to get caught up and concentrate on playing and loose track of time. Taking regular breaks, pause, move, stretch, drink water and take note of any built up tensions. Resting and changing position will help prevent nerve compression & tendinitis. 4. Strengthen up It is beneficial to strengthen particular muscles which work to position the arm and hold the instrument with aim to preventing injury. Bring your instrument into clinic (if possible), and we can customise a strengthening program to suit you and how you play. Carpal Tunnel Syndrome is the name given to a condition where the nerve that travels through the wrist (the Median Nerve) is compressed. The tunnel in the wrist that the nerve travels through is called the Carpal Tunnel.
The nerve can be compressed by surrounding soft tissues (such as swollen tendons), a tight 'roof' to the tunnel (ligament or retinaculum), or a build up of pressure in the tunnel (fluid) due to hormone changes or other reasons. When there is pressure on the nerve, messages can not travel along the nerve as normal. And this is what results in the symptoms associated with carpal tunnel syndrome. Dec 2017 Carpal Tunnel Syndrome is the most common nerve compression that we see in the hand therapy clinic.
Symptoms of Carpal Tunnel Syndrome include;
Hand Therapy can help to manage symptoms of Carpal Tunnel Syndrome with excellent outcomes. We will discuss different treatment options available to you. And communicate with your GP our recommendations- which may include referral to a surgical specialist for their opinion. Nov 2017 Trigger finger is most commonly noticed as clicking or catching of the thumb or finger joints when trying to straighten the finger, commonly first thing in the morning. Often accompanied by pain at the base of the fingers / into the palm. And in some cases the inability to straighten their joint without the help of the other hand.
It occurs due to swelling of either of the finger or thumb flexor tendon sheath +/- pulley. Usually in the palm. Usually occurring in females 50-60 years of age and children under 6. The thumb & ring finger of the right hand are the most common digits affected. Trigger finger can be associated with other conditions including; rheumatoid arthritis, osteoarthritis in the hand, diabetes and hypothyroidism. And can be caused by prolonged gripping of hand tools. Trigger fingers are classified depending upon symptoms. Treatment will be determined by severity of symptoms and may include; Education about the condition Splinting and exercises How to best use your hand in daily activities Modifications to tools Cortisone injection benefit many people with Trigger Finger. When symptoms are severe, referral to a hand plastic or orthopaedic surgeon for an opinion is recommended. The shoulder is the most frequently dislocated joint; most commonly occurring in 20-30 year-old men, followed by elderly women.
The shoulder joint is design to allow for maximal movement, however this makes it vulnerable to dislocation. And once it has popped out of joint, it is 50% likely to again. To prevent shoulder dislocation, it is important to strengthen the 4 muscles which maintain shoulder stability; the Rotator Cuff muscles. Their main role is to work together to hold the humeral head (ball) in the shoulder socket. Exercises using a resistance band can be very effective in strengthening the Rotator Cuff, these can be done at the gym (cable tower) or at home (1meter loop of resistance band attached to door knob). Shoulder internal & external rotation as well as abduction exercises should be completed with each arm, 10-15 reps, 3-5 times per day. If you have sustained a shoulder dislocation in the past; taping or bracing can assist to prevent it happening again. Stretching before 'at risk' sports can be beneficial. And we can always assess the quality and strength of scapula movement and muscles, and provide exercises targeted at any specific instabilities that may have occurred. FOOSH or 'fall on the outstretched hand' is a common mechanism for hand & upper limb injury.
The injury sustained will depend on many factors. Age for instance; children are more likely to sustain an elbow dislocation, adults a scaphoid fracture and the elderly a distal radial or Colles fracture. Some injuries which can be sustained from a FOOSH, include; Hand - soft tissue bruising, laceration, swelling Wrist - fracture (Scaphoid, Colles, Smith's, Barton's) - ligament (scapho-lunate, dorsal carpus, TFCC) - dislocation (lunate, perilunate) Elbow - dislocation (Essex-Lopresti) - ligament (medial collateral, lateral collateral) - fracture (radial hand & neck, olecranon, coronoid process) Arm - fracture (distal or proximal humerus, radius, Monteggia, Galeazzi) Shoulder - dislocation (A/C joint) - rotator cuff or labral tear - fracture (clavicle) Treatment will depend upon the injury. In the early stages there may be the need to immobilise or keep still using a splint or sling. Managing swelling & pain is important to prevent unnecessary stiffness. Movements are incorporated when safe. Strengthening and advice to assist getting back to normal hand and arm use ensure the best outcomes. The difference between a good and an excellent outcome following wrist injury comes down more than rest & repair.
Wrist function involves a complex interplay between wrist ligaments & stabilising muscles. And we increasingly understand that proprioceptive ability plays an important role in hand control and injury prevention. Proprioception is the sense of joint position in space. For example; knowing where your is hand even when you aren't looking at it- when you catch a ball or tuck your shirt in. It involves complex communications between the sensory, motor & central nervous systems. And the ability of specific nerve endings to sense & react to different loads, tensions, speed & degrees of movement in our joints. Following injury we usually rest to recover. During this time normal proprioceptive messages are not sent & received, and proprioceptive ability decreases. When movements and use are reintroduced, the wrist can feel uncoordinated. Specifically designed exercises can be used to improve proprioceptive feedback. Exercises we like to use include; balancing a marble on a plate, juggling, throwing a ball against a wall and balancing a slosh pipe. There are also some great apps available. These exercises give immediate feedback and are fun to do! Hagert, E. Proprioception of the Wrist Joint: A Review of Current Concepts and Possible Implications on Rehabilitation of the Wrist. J Hand Therapy. 2010;232-17. It's a bumper season in the Aussie Alps. But along with snow come sprained thumbs, coined Skier's Thumbs, which account for around 10% of all skiing injuries.
The sprain usually occurs at the base of the thumb (the MCPJ), caused by the stock hyperextending the joint usually during a fall. The ligament injured is the ulnar collateral ligament (UCL). In some cases the UCL will pull off a small bony 'avulsion fracture'. The UCL at the MCPJ is essential in providing stability to the thumb. Without it even holding a pen is difficult! A skilled hand therapist or specialist can determine stability by stress testing the joint. And it is always advisable to have an x-ray or diagnostic ultrasound, to determine whether there is a fracture. The severity of the injury will determine the course of treatment. In some cases a fracture might have moved and an operation will be required. In most cases a hand therapist can fix Skier's Thumb by making a thermoplastic splint that will hold the joint in a safe position whilst the ligament +/- bone heals. Taping techniques can also be used during the splint weaning phase, to help get you back to work / sports quickly & safely. And we will always give you exercises to stabilise the soft tissues around the injured, and surrounding joints. Keep those thumb tips safe! I set about pruning my roses yesterday, and so it should not have been a surprise to wake up this morning with pain on the inside of my elbow!
With so many gardening enthusiasts in the hills - at this time of year we tend to see an influx of gardening associated injures. Especially due to pruning and chopping wood! I was quick to realise that I had symptoms indicative of Golfer's Elbow (or Medial Epicondylitis); an overuse injury to the muscles and tendons that bend the fingers & wrist. People experience pain near the bony bump on the inside of the elbow. This pain is usually associated with resisted gripping or wrist bending. In young people, Golfer's Elbow can occur from an injury during club, racket or throwing sports or weight lifting. Or from work duties including hammering, painting & cooking. The symptoms of pain & weakness in gripping result from damage to the muscles and tendons involved. Chronic Golfer's Elbow is far more common, usually occurring in 35-60 year olds following a period of increased use. The involved soft tissues have age and use-related degeneration, making them susceptible to injury. We provisionally diagnose Golfer's Elbow by taking a history of symptoms and conducting clinical tests. Diagnostic ultrasound and MRI are the best tests to confirm diagnosis. We are always mindful to rule out neck issues in diagnosing Golfer's Elbow. As for Tennis Elbow (Lateral Epicondylitis), the best course of treatment is hotly debated in our professional literature. At AHHOT we focus our treatments on decreasing symptoms, whilst maintaining balanced muscle and tendon load in a graded & safe manner. Taking the time to discuss how each individual uses their body in everyday activities, helps us to customise treatments. We even look at work tools or sporting form to assist getting the best outcome from treatment, and with aim to prevent recurrence. So for now, I will take a bit of my own advice, and finish the pruning next weekend! One of the most common finger injuries to occur during ball sports is Mallet finger.
This is when the finger tip is forcefully bent forwards. The tip then doesn't straighten, because the extensor tendon to the finger has become detached. This may or may not include a small bony fracture (avulsion). Mallet finger can also occur without direct force to the tip, which also is not uncommon. Mallet finger injuries are often treated effectively by splinting the tip of the finger straight for 6-8 weeks. Splinting is most comfortably achieved with a small custom made plastic splint which a hand therapist can make. These splints are safe to wear for most work duties and during game play (when covered with firm tape). It is always recommended that an x-ray is taken to see whether there is a bony fracture. When there is a fracture present, which often occurs in ball v's tip Mallet injuries- the splinting time frames may be shorter. Following the period of immobilisation, movements & use of the finger are gradually introduced. We can teach taping techniques for work and sport to support the tendon in this phase. The tendon injury can remain weak for some time, and it is therefore important that movement and use is introduced safely and gradually. If left untreated the Mallet finger may develop what we call a fixed flexion deformity- meaning that the finger permanently becomes stuck in a bent position and can no longer be straightened. The inability to control a finger like that can be annoying; many men complain it gets in the way when reaching to get their wallet out of their pocket. And a permanently bent tip can become a safety risk- as it is not so easy to get it out of harms way. The art and science of hand therapy really come into play treating Mallet finger injuries! "It's just my finger, don't worry about it, it will get better in a few days..!"
A common (and painful) injury in ball sports is the sprained, dislocated and or fractured finger. In the hills we also see these injuries in people working with horses and cattle, when the finger is forcefully pushed against a gate, or in people falling over on slippery paths in winter. Dorsal PIPJ dislocation usually occurs from hyperextension of the middle bone of the finger- stretching the ligaments on the palm side of the joint. In some instances, middle bone of the finger is pushed right out of joint and becomes stuck on top of the longer finger bone. People are often tempted to put their finger back into place themselves. But DIY relocation could harmfully move a fractured bone, or entrap a surrounding tissue in the joint space (e.g. a ligament, nerve or artery). This may lead to longer term pain, stiffness & deformity. We don't need to look far to see examples of retired football players with fingers riddled with arthritis! A sprained finger will be painful, swollen, and discoloured. Applying ice and compression as soon as possible and buddy taping to a neighbouring finger may assist with continued game play. However if the finger is not sitting straight or moving normally it is best to get it x-rayed, as there is likely ligament +/- bony damage. And if left untreated or not treated correctly and early, this injury can get worse over time and result in repeat dislocations, painful joint deformities and possibly surgery. So please don't ignore that finger sprain- it might not get better in a few days! Do you suffer from pain at the base of your thumb?
You are not alone. 1 in 4 women and 1 in 12 men over 70 suffer from osteoarthritis at the base of their thumb! Osteoarthritis is a common cause of pain at the base of the thumb, usually occurring from middle age. Several joints in the hand can be affected by osteoarthritis, however the CMCJ is the most common. OA occurs when the cartilage on the surface of the joints wears away, small bony growths on the side of the joint occur, the joint surfaces come closer together and supportive ligaments become lax. The joint becomes unstable and painful to move or take any force. Hand Therapy can be very helpful in decreasing acute pain by splinting for a few weeks, or by assisting longer term stability with targeted stretching and strengthening exercises. And providing education about the condition, and how best to use your hands in everyday activities to avoid agitation. Some people will benefit from night or day / work splints to help position joints for the longer term. We also work closely with hand plastic and orthopaedic surgeons who can offer operative interventions. We encourage EPC referrals for eligible clients; usually benefiting from 3+ sessions. Biceps tendinitis is swelling of the long head of the biceps tendon at the shoulder.
Sufferers will commonly complain of pain at the front of the shoulder which may radiate down the arm. The pain is often felt at night, and during overhead activities, including marking or throwing a ball, putting the clothes on the line or painting the ceiling. Some people describe clicking or snapping with shoulder movements. And in more advanced cases simply holding an iPad can increase pain. Biceps tendinitis can sideline a football or tennis player- particularly when a muscle imbalance, joint instability or rotator cuff weakness is present. To prevent biceps tendinitis; - avoid long term repetitive overhead activities - warm up before use (sporting practice & game play) - stretch after strengthening biceps and pecs - strengthen upper back & rotator cuff muscles If you get symptoms; - ice for 20 mins, 2-4 hourly during the initial phase or when the area is warm - avoid agitating activities - tape for sport / work support - consult your GP about NSAIDs or cortisone injection Biceps tendinitis is rarely seen in isolation from other shoulder joint issues. It's best to seek thorough assessment by someone in the know- if you have any shoulder issues. There are 3 main nerves to the arm, and over 30 sites that these nerves can become compressed- little wonder the world of nerves always keeps us fascinated!
What is nerve compression? An injury to the nerve where one or more nerves are compressed by another soft tissue or bone. In the upper limb this can occur in the neck, shoulder, arm, elbow, forearm, wrist or hand. And nerves can be compressed in more than one location along their path from neck to finger. What are the symptoms? Nerve compression can result in feelings of pins and needles during the night, or associated with activities or certain body postures. Some people loose strength or dexterity and can drop things or finding doing fiddly things difficult. Finger tips can loose their fuller shape or might produce less sweat making gripping a challenge. Some people notice changes in the colour of their hand and a burning or heavy feeling. How do you get it? There are many different things that can result in nerve compression. Some include; sleeping or resting posture, holding the arm or hand in the same position for a long time, doing the same activity (movements) repetitively, pressure from tools or even jewellery, or it could just be the way your body is built and moves. How can we help? Hand Therapists can assess where the compression is likely occurring, this can be confirmed in most cases with diagnostic ultrasound or nerve conduction studies. By assessing how you use your body we can often determine the reason for the compression. We also give advice and exercise to try to manage the symptoms, and sometimes supportive day or night splints to help address the problem. We also know when it is the right time to consult with other specialists, to ensure optimal timely team treatment. |
Author Jo MarshClick here to edit Archives
March 2020
|



















 RSS Feed
RSS Feed





