Adelaide & Hills HAND THERAPY
|
Providing creative ways of treating our clients is not new at AHHOT. This is because our business has successfully grown by responding innovatively to change and challenge.
Now, more than ever, we are using our creative & problem solving Occupational Therapy brains, to overcome the difficulties the Corona virus has thrown at us in providing a hands on service. Obviously we need to see clients to custom make splints, measure for pressure garments and closely check wounds. However at AHHOT our method of service delievery is through educating a client about what is causing their concern and guiding them through the process of how they can get better. We don't provide repeated passive treatment sessions, because we don't believe this helps our clients get better faster. Much of how we assess, educate and treat can be done online. And at the moment much of what we do MUST be done online. As health professionals it is our responsiblity to advocate for health in our community. And even though the Federal Government currently assesses our services as 'essential' and enourages us to stay open- it is important that we play our part in stopping the spread.
0 Comments
Before I was a hand therapist I made my first every splint, on myself!
I had a wrist ganglion and was intent on practicing on myself before I applied for my first hand therapy position. Here is some information we are commonly asked about in our clinics. And if you are interested- my ganglion story following. What is a ganglion? Ganglion cyst is a non harmful fluid filled lump which often occurs on the back (dorsum) of the wrist. Less commonly they are found next to the radial artery on the front (volar aspect) of the wrist. And they can also occur at other parts of the body. The ganglion cyst fluid has most commonly leaked from a nearby joint. Less commonly ganglions arise from a joint some distance from the ganglion. And in rare instances ganglions have been reported within a nerve. What does a ganglion feel and look like? A ganglion may result in wrist pain. The ganglion itself is not painful, however it can push on surrounding soft tissues such as nerves, tendons or other joints. Although ganglions at the wrist are a common cause of wrist pain, they are not the only cause of wrist pain. And most ganglions do not cause any pain at all! A lot of people have a ganglion in thier wrist and never see or feel it. If you do see a ganglion, is usually looks like a small round or oval lump or ball on the surface of the wrist. The ball may be firm or soft to touch. What can I do to help fix my ganglion? Hand Therapy for ganglion management involves resting the wrist in the best position to avoid the ganglion getting better. We usually use a custom made thermoplastic splint for this. The splint is usually worn over night when you are asleep, splints may also be used during heavier or work tasks or for symptomatic relief. An experienced hand therapist may provide exercises specicially designed to stabilise the ligaments of the wrist. And also treat associated nerve or tendon issues. In some instances a ganglion will reduce in size with this treatment, however this can take time. And in some instances surgery is recommended. Surgery for wrist ganglions Surgery to remove the ganglion can be very successful. The surgery may be relatively simple if the ganglion has a short root and is not farm from the joint that it comes from. However if the root is long and / or the joint is deep, then surgery can become more involved. Your surgeon will likely discuss this with you. It is often recommeded to rest your wrist in a splint for 2-4 weeks after the surgery. And a hand therapist can help with targeted strengthening and graded functional use programs which address the needs according to your specific ganglion and needs. Hand Therapist's ganglion I suspect my wrist ganglion resulted from a wrist injury sustained at netball several years earlier. My ganglion grew and grew until it sat 2 cm out of the back of my hand! I didn't experience any wrist pain. However the ganglion got in the way when pushing myself up from a chiar or doing push ups. Resting it unfortunately didn't work, so I had surgery with a now retired Adelaide Plastic Surgeon. I rested my wrist in the splint I had made myself for 2 weeks and then gradually started moving it. What I didn't do was manage my scar correctly. And I often show this to my clients as an example of why they need to manage their scars according to hand therapist recommendations! Repetitive Strain Injury (RSI) at the wrist is common and can involve nagging and ongoing pain.
Treating RSI is often not a simple fix, it involves a multifaceted approach. Passive treatment techniques, such as; massage, ultrasound, dry needling, alone rarely get quick results or prevent symptoms from returning. Gaining a good understanding of the problem and cause, is valuable, and often essential, to getting back to doing the things you love quicker and for longer. To help you manage your wrist RSI try the following; Rest Resting the involved area will help prevent overuse and the likely cause of pain. This may involve stopping what you are doing, or slowing down the speed at which you conduct a task. A hand therapist can help to provide you with an orthosis (or splint) which can help to rest your wrist, fingers or thumb- whist still being able to carryout the activites you love. Apply cold Applying cold immediately after an aggitating activity can help to alleviate swelling and pain. Running the area under a cold tap for 5mintues, or applying ice (covered by a towel to avoid direct splin contact) are ways to apply cold. Keep in mind that cold is best used AFTER activity, not during or before. Stretch Stretching out the sore area before, during and after a task which causes aggitation can help. Start by stretching gently, until the amount of stretch would equal a 2/10 feeling of discomfort. Gentle stretch is far more advantageous than forceful stretching, particularly early on and when there is reasonable to significant pain. Stretch can be applied along with heat, stretch with heat will help to lengthen the involved parts. Applying gentle stretch with the palm of your hand is a great way to achieve combination of warmth and stretch. Massage The key to massage when the symptoms are acute (new and most painful), is to massage the area gently yet firmly. The idea of gentle and firm don't seem to go together, but try this; - start by applying a gentle constant pressure over the sore area, - after a minute or so you may try pressing a little furmer on the area, - and then after another minute or so start slowly yet firmly over the area. The warmth and pressure and movement will help the body to recover. Using a roller or rolling a spikey or tennis ball over the area might help once the symptoms settle and the pain has decreased. Having regular massages from a remedial massage therapist is a good way to prevent RSI. It is vital to stay strong even when you are resting the sore area. Maintaining strength through sore muscles and tendons can be achieved with targeted exercises, which won't cause more pain or harm. An experienced hand therapist or physio will know how to keep muscles strong without aggitating your symptoms. Of vital importance is knowing how your body works and how your body reacts to certain tasks and positions. This understanding will help you to keep doing the things you love, whilst letting the RSI heal. Do see the opinion of an Accredited and Certified Hand Therapist who will take the time to listen to how you use your body and recommend alternative methods or equipment to help during your recovery from wrist RSI. For more see our blog on , How to prevent RSI, Prune in June pay for it in July. Preventing musician RSI, Gamer's thumb. RSI or repetitive strain injury is the name given to a number of injuries which can occur with repetitive use of a body part.
Most moving parts of the body can get RSI. Hand therapists most often treat wrist RSI. Symptoms of RSI The symptoms of RSI are varied and multiple. Symptoms may be specific to the part of the body or the structure at that part which is involved. For example overloading of a tendon will result in different symptoms to a nerve which may be pressed on by firm and overworked muscles. Some symptoms include:
Causes of RSI The primary cause of RSI is repetitive use or overloading of a body part over a prolonged period of time. Other causes can include;
See other blogs for some information about different types of RSI. Nerve compression, Biceps tendonitis and how to prevent it, Prune in June and pay for it in July, Do I have carpal tunney syndrome, What is carpal tunnel syndrome, How to prevent musicians RSI, Gamers thumb, Golfer's elbow, Manual workers with carpal tunnel syndrome, Tennis elbow- does a strap help? RSI or repetitive strain injury, as the name suggests, usually results from cumulative trauma over time, as a result of repetitive movements/loads or demands. This is often work related, or related to a recent change in the way the body is required to move during specific tasks.
Preventing RSI from developing or getting worse can be difficult if the cause is work related, or due to an activity which is required (e.g breast feeding). The main way to decrease the risk of getting RSI or making a niggling repetitive strain injury worse is to identify the risky cause or movement and stop or change the way the activity is being done. Often the activity can not be stopped, or the intensity can not be changed (common for self-employedmanual workers). In these cases, there are still things that can be done to minimise the risk of developing RSI, these include; Take regular rest breaks Including regular breaks during repetitive tasks can help. Try setting an alarm to help remind youself to stop and take a break. Down tools or change position Putting down tools or getting up from the desk/chair and standing up or walking around for a few minutes will decrease or change the load, and get the muscles and tendons moving in different ways. Stretch and warm up Stretching and warming up the main muscle groups which are working hard during repetitive tasks is key to helping prevent RSI. Start by stretching and warming up before carrying out tasks; stretch the muscles which will be used a lot and applying warmth with the palm of your hand will ready your body for work. It is important to stretch during the activity/work day, taking time for micro pauses to stretch is a great way to prevent injury and RSI. And retretching at the endof the work day or specific demanding task will also help to prevent the muscles from cooling down quickly and possibly being injured. Stretch the elbows our straight, stretch the wrist in each direction, extend your back, move head side to side- your hand therapist will be able to advise depending upon the repetitive tasks you do. Take care of your whole self Taking care of your general overall health is useful in preventing RSI. This includes drinking plenty of water, eating well and making sure you get regular exercise and avoid habits which are known to cause disease such as smoking cigarettes. Keep you eye on our blog box for our series about RSI, and wrist RSI. And see our other blogs; manual workers, musicians, gamers thumb, golfers elbow, golfers elbow, does a tennis elbow strap help? And you-tube clip for breast feeding mothers. Congratulations are in order!
Our Hand Therapist, Jo Marsh, has successfuly completed the recertification process as a Certified Hand Therapist (CHT). Five years after being titled a Certified Hand Therapist, and over 200 hours of professional development and contribution to the profession of hand therapy later- Jo has recertified. The hand theray certification and the recertification process ensures clients that a therapist with the CHT title continues to develop their specialist skills and practice to a high level treating hand, wrist, elbow and shoulder injuries. When not with clients, Jo's involvement in hand therapy does not stop; "I lecture Masters of OT students in Hand Therapy, informally mentor, I attend conferences & courses about hand therapy as often as I can in Australia and internationally, participate in courses, and present to colleagues findings of my research, read our journal publications and engage with hand therapy and hand surgery colleagues on different platforms". Jo practices in her own rooms in Stirling, and visits Mount Barker and Rose Park for weekly clinics, 8339 HAND (8339 4263). At AHHOT we are proud to have reached the milestone of 3000 days of medical care donated to underprivileged children in India.
Continuing the tradition of local and not so local giving, founding hand therapist Jo Marsh believes in doing business for good every day; "For every appointment we donate a day of medical care for an underprivileged child in India. And for every family or friend referral- we donate a week of medical care for a child in India!" Jo volunteered in Bhutanese refugee camps in Nepal during a long travelling trip to Nepal and India as a new graduate Occupational Therapist. During this time she saw first hand the impact that a lack of funding had on the health of children & young adults. She spend her weeks volunteering with programs specifically for seating with young disabled children, activity building for blind women and program development to decrease STD and unwanted pregnancy in Bhutanese refugee girls. In setting up her own business years later- Jo was determined to give back, not only to the local community- but to those further away. Joining B1G1 and simply buying a day of medical care for every appointment, she is slowly but surely helping to use her business for good. "It is incredible how quickly the days add up. And it feels great! Clients love to know they are also helping to contribute to others. And together we are helping more and more day by day." To learn more about B1G1- business for good go to www.b1g1.com/businessforgood/ Assistive Technology is a device or system that enables a person to perform daily or work tasts that they would otherwise be unable to do. Assistive Technology (or AT) can also be something that makes a task easier or increases safety when performing a task.
Assistive Technology may be something seemingly simple, like a built up pencil grip or non-slip mat. It may also be something more complex like voice recognition to turn on the bedroom lights. The NDIS has listed categories of assistive technology ranging from basic, through standard, specialised and complex. The category of the item will depend upon how readily avaliable it is, whether it requires modification or customisation, how much the item costs, and whether there is any risk involved in using the AT. The NDIS fund AT supports when allocation of funding is made in the current NDIS plan. The level of complexity and degree of cost and potential risk of the item, will depend upon how they are acessed. Low risk and low cost items can be purchased without special forms being completed. However most items require assessment by an AT Assessor with relevant experience involving the item being sought / modified. Our Occupational Therapist is a registered NDIS provider and AT assessor for several items. We are happy to discuss how we might help you access the Assistive Technology that you require through the NDIS, 08 8339 HAND (4263). In our clinic this winter we noticed an increased number of women footballers coming in with injured fingers.
Usually these injuries occur from football v tip (sudden hyperextension) or tackling (rotation and hyperextension). Most common injuries have been volar plate injuries (+/- avulsion fractures). That is, damaging the middle joint (PIPJ) on the palm side of the hand. A few have arrived late having been buddy taped without success. Buddy taping a volar plate injury will ususally not allow for quick healing and delay return to play.
Footy code (locally) enables play when plastic splint is fully covered with tape- we will usually have a splint for sport and another for the rest of the time. We are encouraging early referral so we can get them moving within safe limits immediately. Whilst enabling repair and preventing deformity. The term Accredited Hand Therapist (AHT) is the name given to a practitioner of Hand Therapy who meets specific criterial listed below;
The AHTA is the professional association in Australia which represents Practitioners of Hand Therapy. The association supports it's members by building upon public awareness of the speciality of Hand Therapy through netowrking and representation. And provides professional development oportunities through education and courses and mentorship support. A Certified Hand Therapist (CHT) has internally recognised specialist hand & upper limb rehabilitation skills. To be titled as a CHT an individual must;
There are almost 6600 CHT's world wide, and over 180 in Australia and New Zealand. 85% of CHT's are Occupational Therapists. Choosing a CHT means you are chosing a professional who has demonstrated a high level of knowledge about how the hand & upper limb (fingertip to shoulder) usually are, and how injuries and conditions impact upon the upper limb and how it functions. 1 in 3-4 women over 50 years of age will get osteoarthrtitis (OA) at the base of their thumb. The incidence is less for men, however the symtoms & cause are the same.
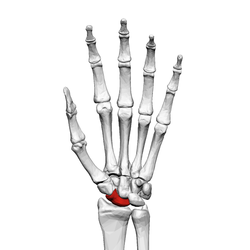
OA is a degenerative joint condition which commonly results is pain, sometimes swelling and decreased movement at a joint. It can result from previous trauma to the joint, or due to chemical changes in the joint, which change the joint surface and surrounding tissues over time. Painful OA is particularly common at the base of the thumb. The joint at the base of the thumb (at the thumb side of the wrist) is called the first carpometacarpal joint (CMCJ). This joint is affected by OA as the joint allows for a complex and wide degree of movements. It is the joint responsible for opposition, where by our thumb pulp (fleshy surface) can face and pinch the finger tip pulps. Because it allows for a great degree of movment, the joint relies on the soft tissues around it to give it stability. However when OA is present, the stability of these structures is often compromised. Throughout our lives the first CMCJ certainly gets a work out! The joint positions the thumb so we can use it in almost all activities involving our hands. And it also absorbes and transfers pressure associated with the forces involved in pinch. These shearing and loading forces are generally well tolerated. This is because the soft tissues (ligaments, tendons, muscles) aroud the joint stabilise it- that is until they are damaged. OA effects change on the bone as well as soft tissues around the involved joint. With loosening and deterioration of the capsule and ligaments around the joint- the bones can shift out of alignment. And this is the process of the development of joint deformities in thumb osteoarthritis. There are different patterns of joint deformity which result from imbalances in muscle and ligament strength and the way the bones line up during different activities. How we can help you, is be assessing the pattern of deformity, seeing which structures are loose and which are tight, and how the bone is shifting during use and sitting at rest. Hand Therapy can help to reposition the joint, and bring balance to the structures which destabilise the thumb. Please call us today so we can help you get the most out of your thumb 08 8339 HAND (8339 4263). Following hand injury sensitivity to cold, or cold intolerance is not uncommon. In fact around 40% of those suffering hand trauma will experience cold intolerance (Novak & McCabe, 2015).
Cold intolerance is more than the usual feelings of chill. Symptoms include ache or pain in and around the injured part. The feeling is excessive to what would usually be expected following exposure to the cold. And in some cases can be severe and result in stiffness. Change in colour of the finger or hand to blue, red or whiter can also occur. Symptoms usually persist until or after the hand is warmed. The exact cause of cold intolerance is unknown. Some research suggests it is more likely following injury to a nerve in the hand (Median or combination Median and Ulnar nerves), +/- damage to a blood vessel. This same research concluded that blunt injury was also more likely to cause issues tolerating the cold (Irwin et al 1997). Other studies have researched cold intolerance following tendon and bone injuries in the hand. Exposure to cold air is the usual trigger, which makes those living and working in cold environments more susceptible. And most research concludes that those who smoke and injury severity are the main predictors of a poor outcome. What can I do to stop cold intolerance? Preventing the fingers / hands getting cold seems to be the only real way of managing cold intolerance. Avoiding exposure to cold air appears to be the best solution for minimising the impact of cold intolerance. And where the temperature can not be controlled using good quality gloves made of natural materials can help. Donning the gloves before leaving the house or car, of before entering the cold environment can help - as warming hands once cold can take time and be painful. A hand therapist or occupational therapist can provide advice about tool handles / grips and other tricks to minimise exposure and the onset of symptoms. In the first instance- avoid cold and don good quality gloves! The scaphoid is one of the carpal bones of the wrist joint.
Scaphoid fractures usually occur following a fall on the outstretched hand. A fracture can occur at differing locations and differing patterns in the bone including; the tubercle, the waist and the proximal pole. Healing of the scaphoid following fracture can take longer than other fractures. This is because the blood supply to the bone is easily disrupted following fracture. And even if a fracture is not seen on x-ray, blood flow can be interrupted. Which may result in ongoing pain and discomfort particularly in forceful gripping tasks. Management of scaphoid fractures requires close and repeated radiographical assessment. And immobilisation in a custom-made cast is required to keep the bones well supported and still such that they can heal. Proximal pole scaphoid fractures Proximal pole fractures account for 10-20% of scaphoid fractures. If left untreated they have a high rate of non-union, that is not healing. Without healing, the blood flow to the bone can be compromised, which results in death or necrosis of the bone. This will almost certainly lead to a painful wrist and over time a change in the way the wrist bones and ligaments work together- and ultimately osteoarthritic changes. Proximal pole fractures are not always seen on x-ray. Therefore, if we have a reasonable degree of suspicion of proximal pole fracture we will always refer back to the treating GP for further radiographical examination. Non-operative management of proximal pole of the scaphoid fractures is unlikely going to be successful- hence we always recommend early referral to a Plastic or Orthopaedic surgeon who is experienced in carpal bone surgery. Surgery usually involves the insertion of a screw to stabilise the fracture and often a k-wire- which will be removed within the first couple of months following surgery. Immobilisation in a custom-made thermoplastic splint is required for several weeks. Managing swelling, scar formation and splint position is the role of the hand therapist. We have tricks to help maintain strength in the hand whilst it is resting in the splint. And as the bone is healed help you regain strength and function once the bone is well healed. The take home message here is: if you are diagnosed with a proximal pole of the scaphoid fracture- it is best to seek early surgical opinion. Scaring from traumatic injury can pose a reminder of unwanted memories. Research suggests scars on the hand & arm are particularly difficult for people to accept, as they can be repeatedly seen throughout the day by the person who suffered them. Reminders of injury and altered appearance can result in negative emotions that limit people to achieve their best. Minimising the appearance and impact of scars is an important role of therapists and surgeons who in the field of burns, plastics & reconstruction.
Therapists employ non-operative techniques which help decrease the size and appearance of scars as they change over time. Discomfort, itchiness and decreased joint movement can also be improved with the right approach at the right time. Some techniques burns & plastics therapist employ to manage scars include; Hydrate & mobilise the scar Frequent application of an oily cream to the scar via firm massage can help minimise the scar height, thickness and itchiness. Scar massage and hydration is required at regular intervals to optimise outcomes. Scar massage helps maintain pliability and movement of the scar around joints or underlying tissues. Contact media Silicon contact media can also help to hydrate the scar, which can result in a flatter, smoother and paler coloured scar. It is believed that applying appropriate silicon products to the scar for a prescribed time frame, can decrease evaporation of moisture through the scar, which in turn may slow down the production of scar within the scar bed. Apply compression Some scars can become raised or thickened over time, specifically deeper scars and burns. The application of pressure over the scar in the form of a compression garment can help to flatten a scar as it changes over time. Compression is especially required for hypertrophic, keloid and full thickness burns scars. Splinting & exercise Most scars will contract, that is get smaller, over time. This can also result in skin contractures, which can limit movement and function. Splinting and exercises can be used to maintain joint range of movement. Preventing skin contracture due to scarring early is far better than trying to fix the problem once it has occurred. Therapists work closely with Plastic & Reconstrucitve Surgeons to obtain optimal outcomes for clients. Surgeons employ other techniques to help minimise the appearance and impact of scars, these include injecting corticosteroid into the scar and various operative techniques. Along with sustaining a deep scar can come a emotional and psychological hurt- talking this through with the right professional can help to overcome the trauma. And working together with a hand therapist to help manage the appearance of scars can have a positive impact on outcomes all round! The Scaphoid is one of the eight carpal bones in the wrist. The carpal bones make up two rows, the Scaphoid is the only which bridges the rows, which puts it at risk of failure (break) due to sudden trauma.
Scaphoid fractures are usually caused by a fall on the outstretched hand (FOOSH). And most often in young adult men in their late teens and 20's(https://www.ncbi.nlm.nih.gov/pubmed/27143737). And most come in following FOOSH during sports (football, snowboarding, trail bike riding). It is not uncommon for a Scaphoid fracture to be missed on early x-ray. Where there is a degree of suspicion of a Scaphoid fracture- repeat x-ray within a few weeks is strongly recommended. This is because the bone has a precarious blood supply, and even with slight change in alignment- this can be disrupted. If not diagnosed and managed appropriate early, lack of blood to part of the bone can result in bone death (necrosis). Which may result in ongoing wrist pain and degenerative changes, which may require surgery. Symptoms Ongoing pain on the thumb side of the wrist can be noticed immediately, and in some instances increase with time. It is not uncommon for people to think they have sprained their wrist, because swelling and bruising may be minor, and they may still have good movement. Treatment Will be determined by whether the fracture has moved bone. If the bone is aligned very well (non-displaced), a firm custom made plastic or plaster cast can be used to support the injured wrist in appropriate alignment until the fracture has healed (6 weeks). However if there is displacement at the fracture site surgical opinion is essential. Surgical fixation of the fracture will involve the use of a screw or pins. If necrosis of bone has occurred, a bone graft may be used to recreate the Scaphoid bone. A plastic or plaster cast will be used to hold the wrist still for 4-6 weeks. And scar management is required. Following removal of the cast a graded strengthening program is required to safely return to sport and working activities. We all have a scar somewhere on our body.
Scarring is a natural process that the body undergoes when healing from a wound. On the skin, scar tissue is mostly made of collagen. The collagen is a protein which is produced to close the edges of a wound to protect us from infection. Hypertrophic and keloid scar tissue sometimes forms when wound healing is delayed and / or excessive collagen is produced. This more likely occurs when there is damage to the deeper layers of skin or following an infection. The excess collagen production results in a scar becoming raised, thick and often darker than the surrounding skin. These scars are not dangerous, however can cause discomfort and limit movement. And for some people had a negative psychological impact. Hypertrophic scar Hypertrophic scars are thick, hard, raised, can be smooth or rough and are frequently darker than the surrounding skin (pink to deep purple). They often occur following a deep cut (laceration), surgical scar or burn. Hypertrophic scars are most likely to form over mobile joints where the skin is required to stretch and move as the joint below changes position. Keloid scar A keloid scar differs from other scars in that it exceeds the border of the original wound. That is, it grows larger than the initial area of injury. These scars are always dark, raised and thick, they can be rubbery, shiny and may be itchy and are sometimes even painful. Keloid scars often result from the site of a pimple, insect bite or piercing. The good news is that there are strategies to help manage the way a scar grows and matures. Seeking guidance from a professional who has experience in burns & scar management will get you set with what you can do to help minimise the appearance of your scar. We know that elbow pain can result from common causes such as a broken bone, tendinitis and arthritis. But when a child or teen report having a sore elbow after sport, without incidence of sudden trauma - the cause may not seem so clear. It is worth investigating whether they have developed Osteochontritis dissecans.
What is Osteochondritis Dissecans? Elbow Osteochondritis dissecans is a condition at the elbow joint, where bone under the cartilage dies due to lack of blood flow. The bone & cartilage become damaged which results in pain and decreased movement at the joint. This may result sudden injury and fracture (like a fall on the outstretched hand). Or from damage to the bone from repetitive trauma (for example during participation in sporting activities particularly involving throwing actions). Symptoms of Osteochondritis dissecans include:
Diagnosis of Osteochondritis dissecans: If you think you or your child may have developed Osteochondritis dissecans it is best to book an appointment to discuss with your doctor. As diagnosis is usually made from reviewing x-ray or MRI of the involved elbow. Treatment for Osteochondritis dissecans: Treatment is determined by the degree of damage to the bone. In some instances, symptoms can be managed without operation with hand therapy alone. However often surgical advice is recommended, as an operation may be required to remove any bone fragment from the joint. Many physios, hand therapists and surgeons recommend an elbow strap or counter-force brace to help manage the symptoms of Lateral Epicondylitis or Tennis Elbow.
But does an elbow strap actually help Tennis Elbow? The simple answer is yes, it can. And there is research to back this up, click here to read. This article published in the Journal of Orthopaedic & Sports Physical Therapy 2009 concludes that use of an elbow strap produced 16% more pain-free grip strength when compared with the use of a placebo or a wrist splint. How does an elbow strap work? Wearing an elbow strap just below the elbow, in theory, takes some of the load off the damaged tendons at the elbow. Put simply;
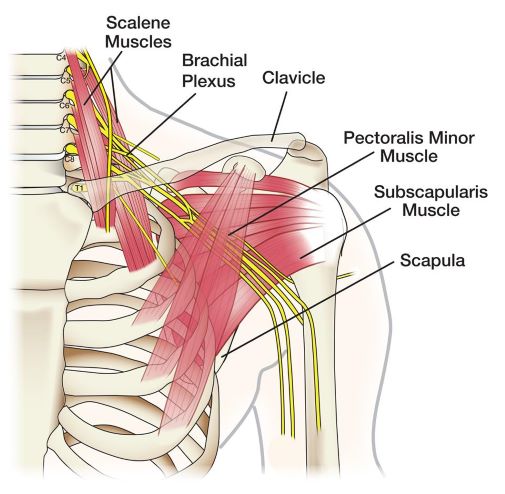
But be warned... There is no guarantee that using an elbow strap for tennis elbow will help! The overall resounding message from the research surrounding non-operative treatment of tennis elbow is- that there is no consensus about what works and does not work! And, in fact, if used incorrectly or for prolonged periods of time, counter-force braces can cause unwanted issues, including compression of the Radial Nerve. So, whats the take home message? Taking load off the tendons will decrease symptoms in tennis elbow- now that's the golden nugget! For other golden nuggets - follow this blog space! What is the Brachial Plexus?
The Brachial Plexus is the name given to the network of nerves as they leave the neck on the way to servicing the shoulder, arm and hand. These nerves are responsible for all shoulder, elbow, wrist and hand movements as well as feeling to these areas. Nerve also also have other functions such as sweating, getting goose bumps & hairs standing up when you are cold and knowing where your joints are positioned- even when you can't see them. What is a Brachial Plexus injury? Injury to the Brachial Plexus is when there is a change in the normal continuity of a part of a nerve or several nerves in the Brachial Plexus. The damage to the nerve results in disruption or stopping of the nerve messages as they travel from the spinal cord to the arm. Symptoms of Brachial Plexus Injury As a result of the messages being blocked or stopped the muscle will not get usual messages from the brain. And without the usual messages from the brain, the muscles will not be able to move properly; they may be weak or lack movement all together. In the same way (but back to front) the messages that our skin give us about feeling; temperature, vibration, texture, will not get to the brain as usual. As the messages from the skin won't be able to travel along injured parts of the nerve where the damage has occurred. Therefore, following Brachial Plexus Injury a person will likely have altered, decreased or no feeling in the part of the arm that is usually serviced by the nerves that are damaged. People may experience other symptoms as a result of nerve damage, including; decreased sweat, and therefore slippery hands which can lead to dropping items. Or when it is cold notice a lack of goosebumps and the hairs not standing up. Hair and nail growth in the injured arm and hand may change. And sometimes the involved hand can look a different colour to the other, for example a mottled appearance, or paler or more blue or red in tone. Types of Brachial Plexus injury Damage to the Brachial Plexus can occur due to a traumatic injury or non-traumatic damage;
Some injuries are transient, that is, symptoms are temporary and full recovery will be anticipated within weeks to months. Other injuries will result in permanent loss of movement and feeling to some or all upper limb muscles, leaving operation/s the only option to regain movement. Operative Carpal Tunnel Release is the procedure used to relieve the symptoms of Carpal Tunnel Syndrome, that is releasing pressure on the median nerve at the level of the wrist. There are two types of surgery commonly performed; endoscopic and open. Both procedures involve cutting the roof of the carpal tunnel, the Transverse Ligament.
Endoscopic Release During Endoscopic surgery the surgeon sees and releases the ligament through a tube which is inserted through a small incision. Following the procedure clients are rarely referred for hand therapy. Open Carpal Tunnel Release Open Carpal Tunnel surgery involves release of the ligament through an incision at the wrist. Open Carpal Tunnel release is especially effective where there is a build up of synovitis or thick fluid or scarring in the carpal tunnel. The open approach allows the surgeon adequate access to the synovitis, such that s/he can remove it. After your Open Carpal Tunnel Release Following this open technique you may wake to find your hand heavily bandaged up, and you may not be able to move your wrist much in these heavy dressings. Stitches are usually removed 10-14 days after the operation. Some people find that their wound opens up in the days following the operation. It is best to discuss this with your surgeon or his/her nurse. If there is no infection present, some wound opening is not usually a concern. Your surgeon, nurse or hand therapist can help to assess and manage wounds. Some people may notice bruising in their palm, this is not usually anything to be concerned about, gently massaging over the bruise may help to settle it. Swelling is also not uncommon after an operation. Hand Therapy can help to manage swelling. Seeking hand therapy assistance early can help get on top of the symptoms early and get you back to using your hand in a timely fashion. Wrist stiffness is also expected when you have been bandaged up. But if stiffness is present in the fingers, thumb, elbow or persists in the wrist- it is recommended you see a hand therapist for assessment of this and advice on how to regain movement. As our hands play such an important role in performing everyday tasks, and many people require the use of their hands for work and hobbies, it can be daunting knowing when is the best time to get back to safely doing certain activities. Our Hand Therapists can help you to regain strength and advise on what tasks are safe to and best to avoid at different time frames following your operation. We can also discuss strategies that can help when you return to work tasks and hobbies which require forceful gripping. We can look at adapting tools, use of specific gloves or splints, and altering the way your body is positioned or moves in specific activities to best protect the operation site. Some people find that they continue to use the strategies they adopt following carpal tunnel release, because they may help reduce recurrence. Carpal Tunnel Release is a relatively common operation, and recovery is usually relatively smooth and straightforward. But if you require a helping hand getting back to doing the things that you most enjoy, a hand therapist can help get you back on track quickly. The following are ways in which the young manual worker can help to manage symptoms of Carpal Tunnel Syndrome during everyday activities and work.
These steps don't offer the magic cure that is so commonly sought after. But those who employ the principals; may well find they are rewarded, and possibly avoid an operation. Carpal Tunnel Syndrome occurs when a nerve (the Median Nerve) is compressed by the structures that surround it as it passes through the Carpal Tunnel (in the wrist). In younger clients who work hard with their hands this is due to;
Some ways to help manage these symptoms include;
Following operative release for Dupuytren's contracture it is not uncommon to experience; swelling, scars, stiffness and some pain in the operated hand.
Most surgical techniques for Dupuytren's Disease involve many precise surgical incisions to remove the diseased tissues. With this amount of work in the palm and fingers, it is not surprising the hand can be uncomfortable to move and use afterwards. To get the best results from your operation, following these simple steps should help; Rest For the first 10-14 days following the operation most people will have stitches holding their skin together. Disrupting wounds early can result in infection, excess scaring and skin breakdown. During this time, unless advised by your surgeon or hand therapist, it is best to keep your hand rested and dressings clean and dry. For the swelling To help bring down the swelling, try elevating your operated hand. It may also help to gently raising your heart rate (walking around the room lifting knees up) whilst raising your arm. Your hand therapist may recommend a gentle form of pressure over the hand and fingers to help manage swelling, for example a lycra glove or compression bandage. For some people, medications and the operative technique may direct how swelling is to be managed, it's best to ask your surgeon whether you have any special precautions. Move early Safe early movement under the direction and observation of the hand surgeon or therapist can help prevent finger joint stiffness. In the early stages try to regain bending and straightening with your own muscle power. Depending upon your operation, using your other hand to straighten the operated or adjacent fingers or thumb may not be advised. Gentle night extension splinting can be used to help stretch out any tightness in the joints. Scar management Once the wounds are dry and clean and the skin is held together, scar massage can start. Keeping the scars in the palm of the hand and fingers supple is essential to getting the best bending and straightening. Early gentle massage with oily cream over the scars and surrounding skin is often combined with the use of a custom made extension night splint. Your hand therapist may also recommend a compression glove and special silicon gel products to help flatten and smooth the scar. Using the hand Depending upon the climate where you live, your work and hobbies, there may be some activities that are best avoided for the first month to 6 weeks. An experienced hand therapist will be able to discuss with you your individual goals, and make suggestions to help get you back to your valued activities as safely and quickly as possible. Please note; if you experience excessive pain or swelling, stiffness or numbness it is always advisable to seek prompt assessment from your surgeon or treating doctor. A small percent of clients will experience complications following operative management for Dupuytren's contracture. Any complication following hand surgery is best diagnosed quickly. Call us 08 8339 HAND It is important that any lump or bump in your hand or arm is investigated by your doctor.
Commonly, however a lump in the palm of the hand is nothing to be concerned about. A lump in the palm can be the first symptom that people notice of Dupuytren's Disease. Dupuytren's Disease is not dangerous, but it can make using the hand difficult as the disease progresses. Dupuytren's Disease is a condition where thick tissues (fascia) under the skin on the palm contract over time. Initially a lump or nodule in the palm develops, people might feel this or see the skin over the lump puckering. It may be painful to hold onto the golf club, but otherwise non problematic. This may be followed by difficulty straightening the finger (usually the little or ring finger or the thumb). This difficulty is caused by further contracting of the fascia and development of cords or bands into the fingers. These bands make straightening the finger increasingly difficult. People often say it becomes difficult getting something out of their pocket because the ring or little finger get stuck. Or they are embarrassed to shake hands as the fingers stay curled over. The progression from lump in the palm to bent over fingers can occur rapidly or over several months or many years. Dupuytren's disease is more common in men than women, and usually occurs in the sixth decade of life. If you suspect you have Dupuytren's Disease, we recommend discussing your options with a Hand Surgeon. Hand Therapy can not help slow down the progression of the disease. We can, however, help you get the best outcomes following interventions from your Surgeon. Call us 08 8339 HAND |
Author Jo MarshClick here to edit Archives
March 2020
|
























 RSS Feed
RSS Feed





