Adelaide & Hills HAND THERAPY
|
Following hand injury sensitivity to cold, or cold intolerance is not uncommon. In fact around 40% of those suffering hand trauma will experience cold intolerance (Novak & McCabe, 2015).
Cold intolerance is more than the usual feelings of chill. Symptoms include ache or pain in and around the injured part. The feeling is excessive to what would usually be expected following exposure to the cold. And in some cases can be severe and result in stiffness. Change in colour of the finger or hand to blue, red or whiter can also occur. Symptoms usually persist until or after the hand is warmed. The exact cause of cold intolerance is unknown. Some research suggests it is more likely following injury to a nerve in the hand (Median or combination Median and Ulnar nerves), +/- damage to a blood vessel. This same research concluded that blunt injury was also more likely to cause issues tolerating the cold (Irwin et al 1997). Other studies have researched cold intolerance following tendon and bone injuries in the hand. Exposure to cold air is the usual trigger, which makes those living and working in cold environments more susceptible. And most research concludes that those who smoke and injury severity are the main predictors of a poor outcome. What can I do to stop cold intolerance? Preventing the fingers / hands getting cold seems to be the only real way of managing cold intolerance. Avoiding exposure to cold air appears to be the best solution for minimising the impact of cold intolerance. And where the temperature can not be controlled using good quality gloves made of natural materials can help. Donning the gloves before leaving the house or car, of before entering the cold environment can help - as warming hands once cold can take time and be painful. A hand therapist or occupational therapist can provide advice about tool handles / grips and other tricks to minimise exposure and the onset of symptoms. In the first instance- avoid cold and don good quality gloves!
0 Comments
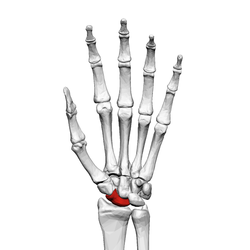
The scaphoid is one of the carpal bones of the wrist joint.
Scaphoid fractures usually occur following a fall on the outstretched hand. A fracture can occur at differing locations and differing patterns in the bone including; the tubercle, the waist and the proximal pole. Healing of the scaphoid following fracture can take longer than other fractures. This is because the blood supply to the bone is easily disrupted following fracture. And even if a fracture is not seen on x-ray, blood flow can be interrupted. Which may result in ongoing pain and discomfort particularly in forceful gripping tasks. Management of scaphoid fractures requires close and repeated radiographical assessment. And immobilisation in a custom-made cast is required to keep the bones well supported and still such that they can heal. Proximal pole scaphoid fractures Proximal pole fractures account for 10-20% of scaphoid fractures. If left untreated they have a high rate of non-union, that is not healing. Without healing, the blood flow to the bone can be compromised, which results in death or necrosis of the bone. This will almost certainly lead to a painful wrist and over time a change in the way the wrist bones and ligaments work together- and ultimately osteoarthritic changes. Proximal pole fractures are not always seen on x-ray. Therefore, if we have a reasonable degree of suspicion of proximal pole fracture we will always refer back to the treating GP for further radiographical examination. Non-operative management of proximal pole of the scaphoid fractures is unlikely going to be successful- hence we always recommend early referral to a Plastic or Orthopaedic surgeon who is experienced in carpal bone surgery. Surgery usually involves the insertion of a screw to stabilise the fracture and often a k-wire- which will be removed within the first couple of months following surgery. Immobilisation in a custom-made thermoplastic splint is required for several weeks. Managing swelling, scar formation and splint position is the role of the hand therapist. We have tricks to help maintain strength in the hand whilst it is resting in the splint. And as the bone is healed help you regain strength and function once the bone is well healed. The take home message here is: if you are diagnosed with a proximal pole of the scaphoid fracture- it is best to seek early surgical opinion. Scaring from traumatic injury can pose a reminder of unwanted memories. Research suggests scars on the hand & arm are particularly difficult for people to accept, as they can be repeatedly seen throughout the day by the person who suffered them. Reminders of injury and altered appearance can result in negative emotions that limit people to achieve their best. Minimising the appearance and impact of scars is an important role of therapists and surgeons who in the field of burns, plastics & reconstruction.
Therapists employ non-operative techniques which help decrease the size and appearance of scars as they change over time. Discomfort, itchiness and decreased joint movement can also be improved with the right approach at the right time. Some techniques burns & plastics therapist employ to manage scars include; Hydrate & mobilise the scar Frequent application of an oily cream to the scar via firm massage can help minimise the scar height, thickness and itchiness. Scar massage and hydration is required at regular intervals to optimise outcomes. Scar massage helps maintain pliability and movement of the scar around joints or underlying tissues. Contact media Silicon contact media can also help to hydrate the scar, which can result in a flatter, smoother and paler coloured scar. It is believed that applying appropriate silicon products to the scar for a prescribed time frame, can decrease evaporation of moisture through the scar, which in turn may slow down the production of scar within the scar bed. Apply compression Some scars can become raised or thickened over time, specifically deeper scars and burns. The application of pressure over the scar in the form of a compression garment can help to flatten a scar as it changes over time. Compression is especially required for hypertrophic, keloid and full thickness burns scars. Splinting & exercise Most scars will contract, that is get smaller, over time. This can also result in skin contractures, which can limit movement and function. Splinting and exercises can be used to maintain joint range of movement. Preventing skin contracture due to scarring early is far better than trying to fix the problem once it has occurred. Therapists work closely with Plastic & Reconstrucitve Surgeons to obtain optimal outcomes for clients. Surgeons employ other techniques to help minimise the appearance and impact of scars, these include injecting corticosteroid into the scar and various operative techniques. Along with sustaining a deep scar can come a emotional and psychological hurt- talking this through with the right professional can help to overcome the trauma. And working together with a hand therapist to help manage the appearance of scars can have a positive impact on outcomes all round! The Scaphoid is one of the eight carpal bones in the wrist. The carpal bones make up two rows, the Scaphoid is the only which bridges the rows, which puts it at risk of failure (break) due to sudden trauma.
Scaphoid fractures are usually caused by a fall on the outstretched hand (FOOSH). And most often in young adult men in their late teens and 20's(https://www.ncbi.nlm.nih.gov/pubmed/27143737). And most come in following FOOSH during sports (football, snowboarding, trail bike riding). It is not uncommon for a Scaphoid fracture to be missed on early x-ray. Where there is a degree of suspicion of a Scaphoid fracture- repeat x-ray within a few weeks is strongly recommended. This is because the bone has a precarious blood supply, and even with slight change in alignment- this can be disrupted. If not diagnosed and managed appropriate early, lack of blood to part of the bone can result in bone death (necrosis). Which may result in ongoing wrist pain and degenerative changes, which may require surgery. Symptoms Ongoing pain on the thumb side of the wrist can be noticed immediately, and in some instances increase with time. It is not uncommon for people to think they have sprained their wrist, because swelling and bruising may be minor, and they may still have good movement. Treatment Will be determined by whether the fracture has moved bone. If the bone is aligned very well (non-displaced), a firm custom made plastic or plaster cast can be used to support the injured wrist in appropriate alignment until the fracture has healed (6 weeks). However if there is displacement at the fracture site surgical opinion is essential. Surgical fixation of the fracture will involve the use of a screw or pins. If necrosis of bone has occurred, a bone graft may be used to recreate the Scaphoid bone. A plastic or plaster cast will be used to hold the wrist still for 4-6 weeks. And scar management is required. Following removal of the cast a graded strengthening program is required to safely return to sport and working activities. |
Author Jo MarshClick here to edit Archives
March 2020
|





 RSS Feed
RSS Feed





